Everything in its right place: understanding and delivering accountable care systems in the NHS

Details
‘Truth is ever to be found in simplicity, and not in the multiplicity and confusion of things’. Isaac Newton
What is an ACS? Why is it different to an ACO?
In March NHS England (NHS E) issued the Five Year Forward View: Next Steps (FYFV:NS) which reviewed the progress made since the original view in 2014 and described a series of steps to support a more joined-up NHS in England. In terms of integrating care the FYFV:NS clarified the next steps for sustainability and transformation plans (STPs) though as partnerships rather than plans. It also set out how accountable care systems (and organisations) might work within this.
STPs started as place-based, multi-year plans built around the needs of local populations – looking to help strengthen local relationships and to bring a shared understanding of the changes necessary to deliver the Five Year Forward View (FYFV). The 44 STPs are at a scale to enable transformation at a pace and level of change to try and meet the conditions of the FYFV. The Next Steps document seeks to rebrand and reboot the STP as a partnership which will all ‘need a basic governance and implementation support chassis to enable effective working’ and which can evolve into its own accountable care system (ACS).
A number of areas across the country had been developing accountable care structures prior to the publication of the FYFV:NS – including vanguards – with a variety of approaches (including governance, contractual and organisational staffing models). Some of these models were also termed accountable care systems (accountable care organisations/partnerships and other titles were also used). The interpretation from the FYFV:NS is slightly different to most of the new care models approaches which are built from the new service/care models rather than an evolution of the STP as a regional planning collaborative.
So what is an accountable care system (ACS) in the current view from NHS England?
Under the FYFV:NS an ACS is now an evolved form of an STP – so it is not a new statutory body and will supplement rather than replace accountabilities of the individual organisations. It may be an STP or part of one (via groups of organisations within an STP sub-area) that is granted more control and freedom over the operation of the local health system for the designated area. This (given the size of some of the 44 STPs) could see multiple ACSs under an STP with delivery via other approaches such as the MCP/PACS and ACO previously outlined in the FYFV and elsewhere.
Importantly for ACS and other emerging care models it is acknowledged that the STP footprint will not cover all planning eventualities – with layers of plans both above and below it. The intent is also not to be prescriptive around organisation form of an ACS (though STPs will not be legal entities/statutory bodies in their own right in any event).
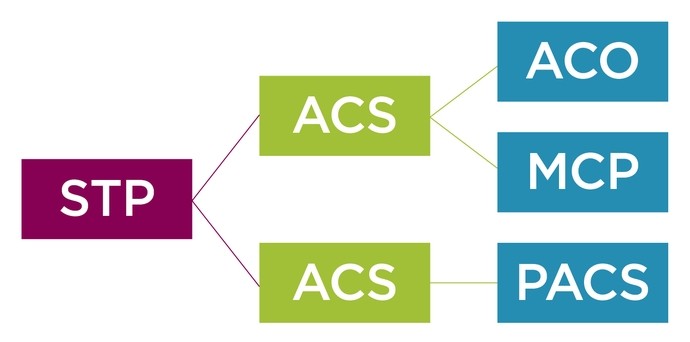
Fig 1: STPs in a local context could flow into multiple ACS which may also have delivery under care models.
‘A locally integrated healthcare system in which both NHS commissioners and providers take on collective responsibility for resources and population health’.
It will be shaped by the relationship between the organisations under the ACS and framed by the ‘accountable performance contract’ with NHSE and NHSI to commit to the targets for the STP and the deliverables of the FYFV:NS. So this ACS is not a delivery mechanism for services but rather a non-statutory forum for organisations to collectively make decisions with shared performance goals and the system ‘control total’. The ACS would not be a new entity and would not hold a services contract so could look along the lines of Figure 2 below.
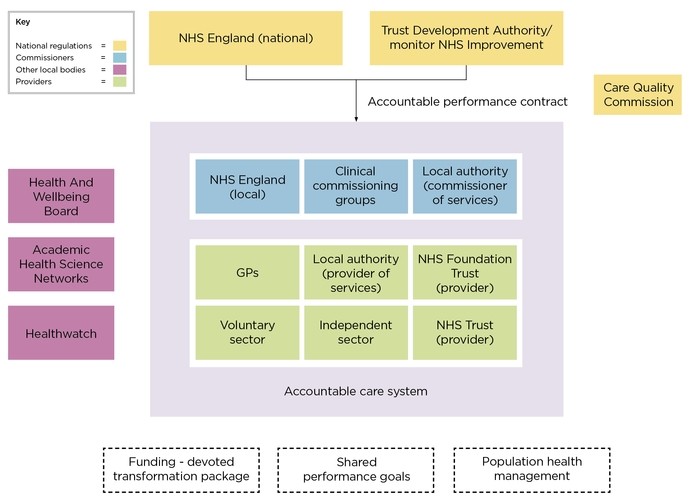
Fig 2: accountable care system approach as an evolved STP
The FYFV:NS looks to bring the emerging accountable care ideas under the umbrella of the wider STP developments which are becoming more solid and influential (despite their lack of legal status). Sustainability and transformation partnerships are a potentially significant shift in a push to wider system-based operation for healthcare organisations and look to deliver on a scale and level which national bodies are demanding in the current stretched financial climate.
It is undeniable that this is all a further step away from the Health and Social Care Act 2012 and the CCG-led commissioning model it created. From a legal position it raises questions and challenges as to how the new thinking can fit the existing legislative framework which envisaged a different ideology of locally based GP-led commissioning with a competitive marketplace of providers.
Contracting for accountable care systems
The intent of the FYFV:NS is that the ACSs should agree an accountable performance contract (APC) with NHSE/NHSI to commit to further improvements and key deliverables. This will therefore be a key document which will need to be signed by a significant number of parties as well as the national regulators.
NHSE and NHSI will be looking for the ACS to sign up to key targets and deliverables for the system. This could incorporate more patient focused outcome measures, in line with the introduction of these models in many new care models approaches nationally already in place.
The APC should also be underpinned by clear collective decision making and governance between the ACS members – setting out how they will operate on a system footprint, how the population-based budget will be managed – how investment and disinvestment will be determined and how they will operate on a more integrated basis.
There should therefore be a separate ACS agreement entered into between the parties to the ACS setting out these mechanisms as well as elements such as:
- designation of the patient population covered by the ACS
- information exchange/governance
- how parties can enter/exit
- how disputes will be resolved
- the agreed core principles for the operation of the ACS
- reviews/change management
There is space within the ‘governance chassis’ for the commissioners to integrate more and to coordinate commissioner decisions and for the providers to collaborate through approaches such as provider alliances.
Importantly the APC and the ACS agreement as described above would not be directly services contracts so will overarch the existing contractual structures without replacing them in a similar manner to how the NHS alliance agreement operates.
This means that commissioners will additionally need to consider their current services contracts and this is where you could start to see an ACP and ACS agreement underpinned by delivery through an MCP contract. This may appear a complex contractual infrastructure to get to the destination point but there are likely to be opportunities for streamlining the contracting infrastructure through reference to common approaches/policies/outcomes in some of the system level documents (APC and ACS).
What does this mean for accountable care organisations?
The commonly used definition of ACOs is as organisation(s) delivering care for a defined population under a capitated budget with actions under a contract with a commissioner. This approach could sit under an ACS (depending on the size of the STP you may have a number of ACOs operating within one larger area – for example if the North Eastern STPs were to come together or within the South Yorkshire STP/ACS).
Given the approach of the draft ACO contract issued by NHS England in August 2017, the contractual/legal vision is for a legal entity to hold the contract with the commissioners and be accountable for the delivery of services to the population. This would keep the commissioners and providers on opposite sides of the ACO contract which could then become the interface between the commissioners and providers for service delivery.
The FYFV:NS does envisage that an ACS could ultimately become an ACO via becoming a single organisation for the commissioners of the area to contract with for health and care/population health in the area. It also states that this may take several years to achieve due to its scale and complexity.
Given the acknowledged complexity of delivering an ACO, save for those areas which are significantly advanced in the process, we would expect to see further MCP structures (including primary care home) and alliances in the shorter term as routes to greater local integrated delivery which link into the wider population coverage of the STP/ACS.
Delivering ACS - how we can help you
We have extensive experience of working on accountable care projects and integration in the health sector. Our broad ranging sector expertise allows us to provide you with tailored legal advice that draws upon current market practice and best practice from around the country.
In particular, we can:
- help to develop the ACS agreement structure: we are working with clients on this and taking the structure beyond the initial memorandum of understanding stage
- advise upon STP, ACS and other project governance structures and appropriate terms of reference
- discuss and advise you on the details of the accountable performance contract with the national regulators and how this fits with the local arrangements between organisations
- advise on structuring internal options appraisals to evaluate delivery model options and any requirements around the ISAP process
- carry out legal due diligence on existing arrangements to understand flexibilities and associated cost
- provide legal advice on the public law duties (including engagement and consultation)
- advise on procurement law and provide a checklist of NHS act duties to ensure commissioning duties are met
- carry out a legal competition assessment of any proposed transaction
- negotiate and draft data sharing agreements to regulate access to relevant patient records and other data
- advising on the application of TUPE or COSOP and associated transaction structuring
- review and advise on board approvals and external regulators
- provide advice regarding strategic use of estate assets






