Part four: Collaborating - what works best for you?

Details
Joint venture or working with your local NHS trust?
In our previous three articles (parts one, two and three) we’ve looked at GPs working together to form ’federations’ and the different ways this can happen. A partnership remains the most common structure used within general practice. In the context of the current changes in the NHS following on from the Five Year Forward View and GP Forward View, the need for GPs to collaborate with each other and other NHS entities across a wider population means that the traditional partnership form may well not deliver the required integration, flexibility and protections for participants and as a result many different organisational forms are being explored.
We considered mergers and the overarching super-partnership structures in our last article and we will now focus on joint ventures and working more closely with NHS trusts, to deliver more integrated services for the benefit of patients and to manage the strains GPs are currently facing within partnerships or single handed practices.
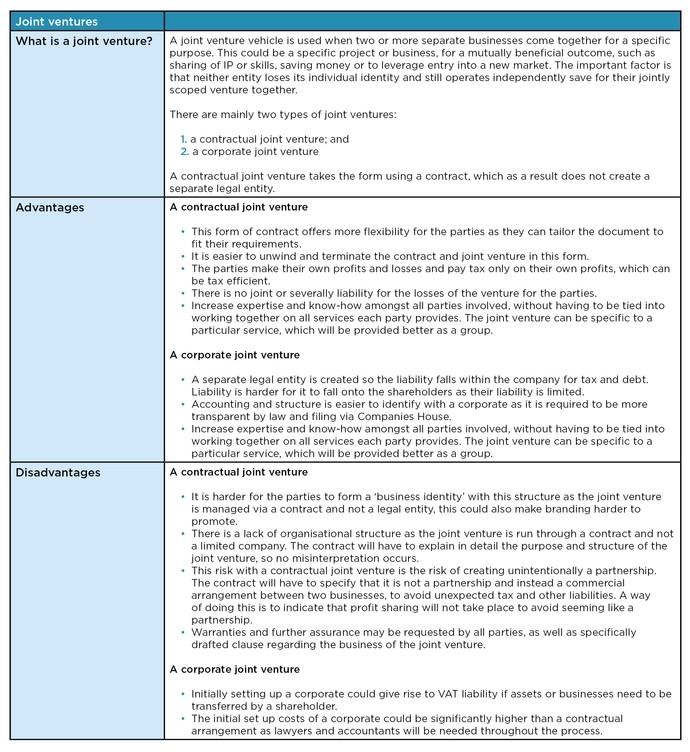
Factors to consider when entering into a joint venture arrangement in the NHS:
- A joint venture can be entered into by individual practices, existing federations and practice mergers. They are seen to be entering into joint ventures with private providers in healthcare as well as other local federations to collaborate on working together.
- Deciding on whether a limited company or a contractual joint venture is set up, could depend on the duration of the service to be provided, who the parties are and their preference for individual organisational reasons.
- A risk for a contractual joint venture is if the governing documents are not drafted correctly there could be no limit to the liability of the parties. Primary care providers with General Medical Services and Personal Medical Services agreements will want to protect their contract and obligations and therefore ring fence these separately to remain within the practice, so they do not form any part of a joint venture.
- NHS trusts have limited ability to form joint venture companies whilst NHS foundation trusts (NHS FT) have more legal capacity to do so but need to comply with regulatory requirements. The parties will need to ensure appropriate internal approvals and that they have complied with the NHS FT’s internal governance arrangements; standing orders and standing financial instructions; external regulatory requirements set by NHSI (such as where they are under special measures).
- Consultation and engagement duties will still need to be considered especially where any employees may be expected to work for the joint venture. Patients will also need to be notified if there is to be a change in patient care as a result of the joint venture.
- Competition and procurement will still apply to the joint venture so for example the parties will need to be aware of the potential obligations to tender for NHS contracts which they may want to award to the joint venture.
Integration into an NHS FT
The pressures encountered within general practice today, have seen many alternative collaboration methods being adopted. One which has been seen as controversial in some areas of the country is the local NHS FT taking over the running of the GP practice. This form of ‘takeover’ has been a work in progress over the last few years, but in recent months we are seeing an increase in GPs open to the idea of their practices being run by a local NHS FT. In these models the GPs can opt to be salaried practitioners at the FT or we have also seen joint venture approaches and new corporate vehicles being formed to house the collaboration.
For new models of place based accountable care to be successful it is important that primary care is heavily involved. If GPs wish to play a key role in these models then they would want to have a clearer voice which is representative of practices in the place. If the vision is that there is one accountable care organisation, the governance arrangements within an FT which might take over GP practices should change accordingly to take on board the role of primary care. This could take the form of primary care representation on the board or executive members, and could also include the possibility of a new primary care division (or even FT owned corporate vehicle). There also needs to be consideration of how any risk share mechanism to be developed around the delivery of the shared outcomes e.g. successfully achieving reduced attendance at A&E or greater care provided in the community or at home than at the start of the collaboration.
Why is this happening?
In our previous articles we highlighted the pressures that are being felt within primary care. The levels of the workforce and the struggle to recruit new GPs especially in more remote areas of the country has increased the burden current GPs and partners are enduring on a day-to-day basis to fulfil their obligations under their contract and still run their practice. The ongoing financial restraints and budget cuts, elsewhere in the system have also resulted in further pressures being added in primary care to provide a good quality of service which can reduce demand in other areas such as A&E.
A number of questions arise with greater NHS FT involvement with primary care, especially if the GPs decide to become salaried. The prospective benefits could include a wider management cost base to deal with the Care Quality Commission (CQC), rising indemnity costs (though we note the GP indemnity proposals) or liability under the GMS/PMS primary care contract they once held. This in the current climate could even be seen as a form of succession planning by the GPs, who believe there will not be a new generation of GPs willing to take over their contract at the point of retirement.
We have also seen some circumstances where an NHS FT has taken over the running of a failing GP practice for an interim period, to save the practice from closing at the behest of the Clinical Commissioning Groups (CCG). These examples further highlight the current precarious nature of some primary care practices at the current time along with areas where GPs have handed back their contracts.
NHS FT based models can assist practices encountering financial pressures, either for an interim period or indefinitely. They can also provide wider organisational capacity for delivering more integrated services and shared back office. However the parties will need to be clear on their expectations, how the governance will work and how the service change will work for patients.
How we can help?
We have developed model documents to assist our clients to form joint ventures no matter which structure you wish to use. For our clients, we have:
- options appraisals with ‘pros and cons’ for the most appropriate structure for you, dependant on the desires and expected outcomes of the joint venture or FT takeover
- tailored advice regarding the corporate structure, governance, board, employment, property, liabilities, procurement and contract reviews
- model articles, board minutes and shareholders agreements should the parties wish to incorporate a new joint venture company, which can easily be tailored to meet your needs
- model joint venture agreement, which we can tailor to meet your needs
- experience in advising in FT takeovers and can guide you through the whole process, from agreeing a MoU to finalising a complete handover of the practice
We are growing our commercial healthcare team and have recruited Christiana Demetriou, Bethany Gore and Ruth Griffiths, who are all experts on primary care issues, corporate forms and federation structures and solving the issues our clients are grappling with around primary care at scale.
Read part one: Collaborating – what works best for you?






