Working through change

Details
The NHS has seen significant reorganisation since forming in 1948 but the last few years in particular have introduced a whole host of new initiatives (and new jargon). From place-based commissioning, population budgets and integrated care delivered through new models of care and accountable care systems/organisations, to the recently renamed Sustainability and Transformation Partnerships (previously ‘plans’).
But what does it all actually mean? What is the difference between them? And how does any of it work in practice? In this article we peel back the layers and look at some of the contracting structures underpinning it all.
Sustainability and transformation - a quick context
Sustainability and transformation plans, the top layer - were first announced by NHS England in the NHS shared planning guidance of December 2015. The planning guidance tasked health and care systems across England with creating five-year plans to set out how areas - regional ‘footprints’ - should implement the three pillars of the NHS England five year forward view; namely closing the health and wellbeing gap, closing the care and quality gap and closing the finance and efficiency gap.
NHS England published its Next Steps on the NHS Five Year Forward View in March 2017 which has renamed the ‘footprints’ as Sustainability and Transformation Partnerships (STPs) and requires the governance and organisational arrangements for STPs to be formalised, including the creation of an STP board.
STPs are not ‘a thing’ as such but a collection of collaborative arrangements and shared governance and decision making processes between multiple organisations, both commissioner and provider side, aimed at ensuring that they all work together and pull in the same direction when it comes to delivery of improved quality of care and integration of the care pathway for patients.
Local plans/systems
There are a variety of smaller scale local arrangements within each regional STP footprint. These include population-based care models such as multispecialty community providers (MCP) and primary and acute care systems (PACS) - (both types of ‘prime provider’ models) - as well as acute care collaborations (ACC) - sometimes referred to as hospital chains. There are also models dealing specifically with enhanced health in care homes (EHCH) and urgent and emergency care. Most recently we have seen the emergence of the primary care home model (PCH), which is a form of MCP; and the acute medical model, which looks at acute
medical services in smaller district hospitals.
Individual organisations will be involved in a variety of different local models/systems and these will integrate with each other to create the larger scale systems (often referred to as integrated or accountable care systems). For example, the acute trust in a PACS may join a hospital group or ACC to support sustainability of acute services over a bigger geography. Some PACS involved in the NHS England vanguard programme (e.g. Salford Together and Northumberland ACO) are establishing hospital groups in this way.
The aim of these integrated or accountable care systems (ICS/ACS) is to deliver population-based care across the area they cover. Some STPs are looking to develop themselves into a single ACS but in many areas the STP footprint is too large for one ACS and the likelihood is that there will be several ACSs in each STP footprint.
Even more advanced is the accountable care organisation (ACO), where individual organisations create an entirely new entity (through merger or otherwise) to deliver all the care for the population in its area. However, it is widely accepted that this is more difficult and current legislative limits on the merging of functions, together with funding constraints and the impact of competition law in the UK mean it is unlikely that this model will gain traction in the near future.
Contracting models
It is always key to ensure that you are absolutely clear with your partners about what you want to achieve before embarking on any major organisational changes - form follows function. Having said that, it is helpful to consider what kinds of models might help you to achieve your aims. Whilst these models will differ in the scope of services and scale that they deliver, in legal terms they are no different. There are just three types of legal structure ranging from the informal to the more formal: a loose contract structure; a contractual joint venture; and new corporate entity.
To understand them better it is useful to look at the three models for MCPs and PACS identified by NHS England:
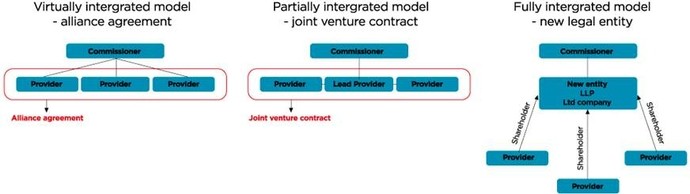
Virtually integrated model
Individual providers are bound together by an ‘alliance’ agreement. This ‘alliance’ agreement is the loose contractual form and is often just a memorandum of understanding. It does not replace traditional commissioning contracts and each provider still holds its own existing commissioning contract. The aim is to improve integration within and between the services they have agreed to develop, without any change to the underlying contracts; for example through shared management of resources, risk sharing agreements and the delivery of services. Decisions between parties are made using a variety of joint committees and committees in common.
Partially integrated model
This involves a more formal arrangement such as a joint venture (JV). The JV could be contractual or a separate corporate entity. The aim would be for the JV to hold a single ‘integrated services’ commissioning contract for all services provided (except any core primary medical services involved which would be covered under a separate contract between GPs and the JV). If the JV is a corporate entity, it would hold the main ‘integrated services’ commissioning contract. If the JV is contractual, one organisation would take a lead contracting role (the ‘prime provider’) and hold the contract for all the organisations. The contractual JV would then outline how each would play their part in service delivery. Again this would be supported by a variety of joint committees/committees in common.
Fully integrated model
This model again could involve a contractual JV, but will most probably require a separate corporate JV entity to achieve the full integration anticipated. The entity holds a single whole-population budget for the full range of services in scope including any primary medical services involved. This is the most complicated option and, therefore, considered the most difficult to achieve.
Whilst not technically a population based care model, a similar three strand approach can be seen in the various types of ACC, which range from hospital networks (e.g. accountable cancer network) through to a hospital chain (e.g. Salford and Wigan Foundation Chain) and even to a full merger (e.g. the Single Hospital Service in Manchester).
How we can help
Hill Dickinson is working with a number of different NHS clients on their integration projects, providing advice and support from the earliest stages of service planning, through public consultation and engagement processes, to formalising risk sharing arrangements and contracting structures.






