Playing the long game: part two

Details
New approaches to the design and operation of NHS bodies following the five year forward view
Part two: challenges in introducing a new system/population approach in the NHS
In the first article of this series we noted that the NHS has and will continue to seek to reinvent itself through wider planning under STPs, developing new models of population based healthcare – redefining the roles of providers and commissioners within accountable care organisations/systems and new forms of collaboration such as alliances within the terms of the current legal framework.
Some of the practical and legal issues which this gives rise to will include how the governance system works and how the contractual collaboration could work.
Breaking through the silos/governance and decision making
Practically the initial operation of the new collaborative models in the NHS will require large numbers of statutory organisations to work together, sometimes taking steps which may be against their immediate organisational interests.
Where this remains a non-binding consensus approach, a key issue is the possibility of each organisation effectively having a veto on collective decisions. Also when decisions become difficult and complex (for example around changes to hospitals/services) then they can be deliberately avoided, become delayed in endless discussions in working groups or the parties may just look to disengage.
Some systems with stronger leadership have managed to progress models through meetings in common and agreeing parallel complementary actions in the absence of having a formal joint decision-making structure (sometimes with a memorandum of understanding). This approach remains dependent on strong relationships between key individuals and can be knocked off-kilter by external financial and regulatory pressures. Further there are some areas where the sheer number of statutory organisations (CCGs, providers and local authorities), different organisational governance structures and complexity of the geographical cross overs between them make managing a population based approach especially complex.
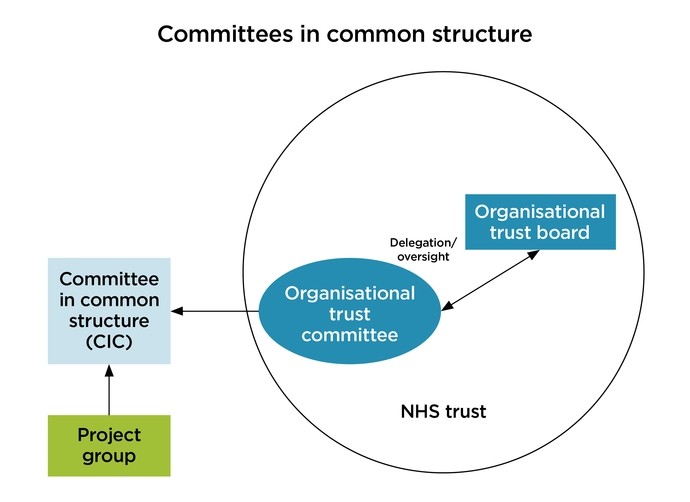
‘Committees in common’, means that organisations remain individually accountable for their decisions. Participants can establish their own internal organisational committees which are committees of their respective boards as a framework for internal oversight of the wider system work. Working agreements (such as terms of reference or a short list of ground rules) are helpful in describing what the organisations expectations are for how the committees will work together.
Any proposed structure will still need to be clear as to which organisation is responsible for specific decisions in the system (and their process for this approval which may include referral to board or council of governors or public engagement in certain circumstances). It would be important to avoid having providers taking decisions which under statute should sit with the CCG, for example.
An approach which is also gaining pace in the NHS is to simplify the debate by reducing the number of organisations which are (actively) involved in the system. This can be through routes such as CCG mergers, trust mergers and acquisitions, common appointments/governing bodies and also delegation of authority between statutory bodies where permitted. The reduction in the number of statutory bodies with duties for a population can make the form of the collaboration simpler and reduce the number of competing interests and the risk of challenges which can delay and derail decision taking. Achieving buy-in from those organisations perceiving a ‘loss of control’ through, for example, lead commissioning arrangements, will remain a challenge.
Appropriate consideration should be given to the attendees for the group, their level of delegation and the reporting structure back to their nominating organisations to ensure accountability and appropriate oversight. This would include non-executives and governors for foundation trusts and governing body/CCG membership for CCGs. Clinical representation is critical.
Contractual collaboration and integration
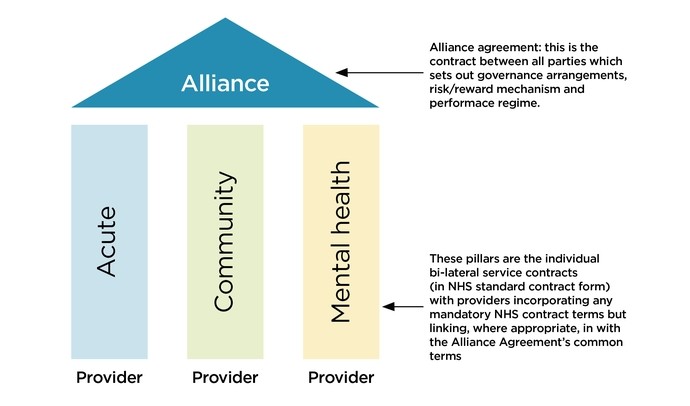
In order to try to move beyond a model based on the personalities of key individuals or lighter non-binding co-operation some areas have sought to align their vision for the local system into a formal contractual relationship such as an alliance agreement. We have seen this approach in areas such as Lambeth and also internationally in Canterbury, New Zealand. The alliance approach seeks to move parties away from their own individual focus towards the collective aims and outcomes so they can sit above and overarch some of the current arrangements.
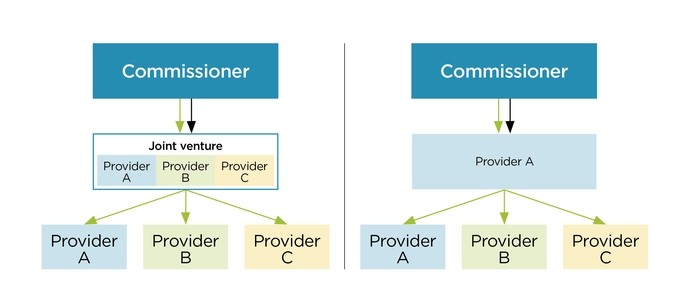
In other areas there have been steps taken to implement a more structured ‘lead provider’ approach to accountable care and system working where you have a sole provider who will liaise with (ideally) an integrated commissioner for the services which it will manage through a network of associated providers/sub-contractors (for example the Salford Integrated Care Organisation). This can increase (or enforce) a greater degree of co-operation across providers and introduce a system integrator role. There are a number of ways in which this lead provider role can operate which vary from the ‘command and control’ model where one provider is managing the system to a more collaborative joint venture between providers underneath the main contract held by a representative provider.
This approach keeps the separation between the commissioner and provider functions, though it is a different approach to have commissioners directly delivering their functions via contracts with providers currently. The future role and method of commissioning in these types of models could see a much lighter CCG with more of the ‘supply chain’ management role sitting within the core provider.
In the final article in this series we will examine some of the other issues in the system redesign such as the blurring of the divide between providers and purchasers, funding models and how the new approach fits within the procurement and competition framework.
Read part one: the organic shift to a system approach
Read part three: challenges in introducing a new system/population approach in the NHS






